Hormone Imbalances and Conditions
Hormones function as the body's chemical messengers, coordinating essential processes from growth and metabolism to reproduction and stress response. When these finely-tuned systems become imbalanced, the effects ripple throughout the body, often manifesting as seemingly unrelated symptoms that can significantly impact quality of life.
Hormone imbalances affect millions of Americans, with women being 5-8 times more likely than men to experience thyroid disorders alone, while testosterone deficiency impacts up to 30% of overweight men. These messengers regulate everything from metabolism to mood, but can become disrupted by aging, stress, environmental toxins, and lifestyle factors, cascading effects throughout the body. Understanding these imbalances and available treatment options has become increasingly important as research reveals the interconnected nature of hormonal systems.
The primary causes of hormone imbalances include the natural aging process, which leads to gradual hormone decline starting as early as the late twenties. Environmental factors play an increasingly significant role, including exposure to heavy metals, chemicals in foods, cosmetics and cleaning products, and blue light pollution that disrupts natural circadian rhythms. Lifestyle factors such as poor sleep hygiene, chronic stress, toxic relationships, and habitual negative thought patterns can further disrupt hormonal balance.
What makes hormone imbalances particularly challenging to diagnose is their interconnected nature. The endocrine system operates as a complex web where dysfunction in one area affects others. For instance, chronic stress elevates cortisol levels, which can suppress thyroid function and disrupt insulin sensitivity, ultimately affecting sex hormone production. This cascade effect explains why addressing foundational hormones like cortisol, insulin, and thyroid often allows sex hormones to naturally rebalance.

Modern testing approaches have evolved beyond basic hormone panels to include comprehensive assessments using blood, urine, and saliva tests that measure not just hormone levels but also their metabolites and the body's ability to utilize these hormones effectively. This broader perspective enables healthcare providers to identify subtle imbalances before they progress to severe dysfunction.
Perimenopause and menopause hormone imbalances
Perimenopause is the pre-menopause transitional period that typically begins in the mid-40s but can start as early as the mid-30s for some women. During this phase, estrogen and progesterone levels fluctuate dramatically and unpredictably, with progesterone declining faster than estrogen, creating an imbalanced ratio that drives many uncomfortable symptoms.
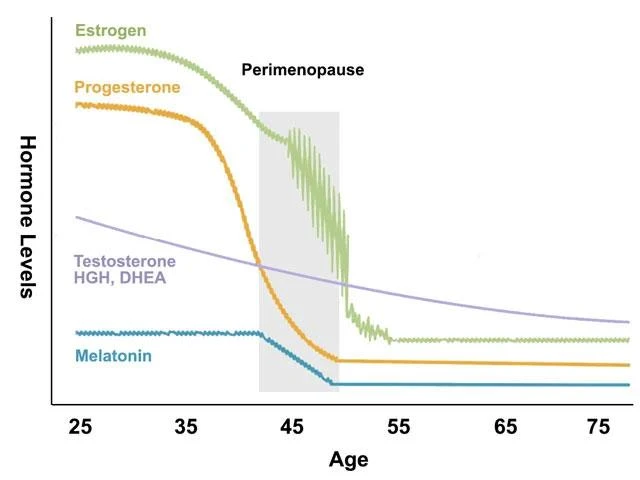
The hormonal changes during perimenopause are characterized by erratic fluctuations rather than steady declines. Estrogen levels can rise and fall dramatically within the same cycle, while progesterone production decreases more consistently. This creates periods of estrogen dominance that contribute to weight gain, mood swings, and menstrual irregularities. The transition can last several years before progressing to menopause, when hormone production essentially ceases.
Physical symptoms include irregular menstrual cycles with periods becoming heavier, lighter, more frequent, or completely skipped. Hot flashes and night sweats affect up to 75% of women, often disrupting sleep quality. Weight gain typically occurs in new areas (particularly the abdomen, arms, and thighs) as metabolic changes accompany hormonal shifts. Joint pain, dry skin and hair, and decreased muscle tone are common as estrogen's protective effects diminish.
Cognitive and emotional symptoms can be particularly distressing. Brain fog and memory issues affect approximately 12% of women clinically, while mood swings, irritability, anxiety, and depression become more frequent. Sleep disturbances extend beyond night sweats to include difficulty falling asleep and staying asleep, creating a cycle of fatigue that compounds other symptoms.

The average age of menopause is 52, but this can be accelerated by factors such as smoking (advancing menopause by 1-2 years), certain medical treatments like chemotherapy and radiation, or surgical removal of the ovaries. Recent research from 2024 shows that modern, lower-dose hormone therapies are significantly safer than older formulations, with studies indicating a 19% reduction in mortality with estrogen-only therapy and significant reductions in breast, lung, and colorectal cancer risks when used appropriately. Bioidentical hormone replacement therapy for estrogen and progesterone can be an effective treatment for perimenopause and menopause symptoms.
Testosterone hormone imbalances
Testosterone deficiency affects both men and women, although the causes and manifestations differ significantly between genders. In men, testosterone levels naturally decline by approximately 1% per year after age 30, with levels below 300 ng/dL combined with symptoms indicating clinical deficiency.
Low testosterone symptoms in men include reduced sexual desire and erectile dysfunction, loss of muscle mass and strength, increased body fat particularly around the midsection, and the development of gynecomastia in some cases. Energy levels plummet, leading to persistent fatigue and decreased motivation. Cognitive symptoms include depression, difficulty concentrating, and memory problems. Physical signs may include hot flashes, mood swings, and night sweats.

Male testosterone deficiency can have many causes, including primary hypogonadism caused by testicular problems such as injury, cancer, or genetic conditions, and secondary hypogonadism resulting from pituitary or hypothalamic dysfunction. Type 2 diabetes is associated with testosterone deficiency in 25% of cases, while obesity increases risk by 30% in overweight men. Chronic illnesses, stress, and sedentary lifestyles further compound the problem.
Current treatment approaches focus on bioidentical hormone replacement when clinically appropriate, although testosterone therapy requires careful monitoring due to potential side effects. Lifestyle interventions including resistance training, adequate sleep, stress management, and maintaining healthy body weight can naturally support testosterone production in both men and women.
Thyroid hormone imbalances
Thyroid disorders affect an estimated 20 million Americans, making them among the most common endocrine conditions. The thyroid system operates through the hypothalamic-pituitary-thyroid axis, where the hypothalamus releases TRH, the pituitary responds with TSH, and the thyroid produces T4 and the more active T3 hormone. The thyroid hormones then affect your metabolism, heart rate, breathing, digestion, fertility, and almost every organ in your body. When your thyroid hormones are out of balance, it can impact your entire body.
Hypothyroidism, the most common thyroid condition, presents with unexplained weight gain or difficulty losing weight, persistent sluggishness and fatigue, brain fog with poor focus and memory, dry skin and hair, cold sensitivity, and heavier, more frequent menstrual periods in women. This condition results from insufficient thyroid hormone production, slowing metabolism and affecting virtually every body system.

Hyperthyroidism, though less common with an overall prevalence of 1.2% in the US, causes rapid weight loss despite increased appetite, fast heart rate, heat intolerance and excessive sweating, anxiety and nervousness, tremors, sleep difficulties, muscle weakness, and irregular menstrual periods. The most common cause is Graves' disease, accounting for approximately 70% of cases.
Hashimoto's disease
Hashimoto's disease represents an autoimmune variant of hypothyroidism where the body's immune system attacks the thyroid gland. This condition is characterized by the production of antibodies against the thyroid (thyroid peroxidase (TPO) and thyroglobulin), leading to the gradual destruction of thyroid tissue. Women are affected 7-10 times more than men, with peak onset occurring between ages 30-50.
The progression of Hashimoto's typically occurs in stages: an early phase that may temporarily cause hyperthyroid symptoms due to hormone release from damaged cells, a gradual progression to hypothyroidism over months to years, and a late stage requiring lifelong hormone replacement therapy. Risk factors include family history of thyroid or autoimmune diseases, other autoimmune conditions like Type 1 diabetes or rheumatoid arthritis, excessive iodine intake, radiation exposure, and certain viral infections.
Diagnostic approaches for Hashimoto's disease have evolved significantly, with TSH serving as the gold standard initial test, followed by free T4 measurement when TSH is abnormal. Specialized testing includes thyroid antibodies (TPO and thyroglobulin antibodies for Hashimoto's, TSH receptor antibodies for Graves' disease), and advanced imaging studies when indicated.
Treatment focuses on addressing both the autoimmune component and thyroid hormone deficiency. This includes reducing autoimmune flare-ups through gut health optimization, addressing environmental triggers like heavy metals and gluten sensitivity, and providing bioidentical thyroid hormones when the gland cannot produce sufficient quantities.
Adrenal hormone imbalances
The adrenal glands, small triangle-shaped organs located atop each kidney, produce critical hormones including cortisol for stress response and metabolism regulation, aldosterone for blood pressure and electrolyte balance, and adrenaline for the fight-or-flight response. These glands operate through the hypothalamic-pituitary-adrenal (HPA) axis, a complex communication system that maintains hormonal homeostasis.
Cortisol dysfunction manifests differently depending on whether levels are too high or too low. High cortisol (hypercortisolism) symptoms include central weight gain with thin extremities, "moon face", purple stretch marks, easy bruising, high blood pressure and blood sugar, muscle weakness, mood changes including depression and irritability, and increased infection susceptibility. This pattern is seen in Cushing's syndrome, which can result from long-term corticosteroid use or tumors producing excess cortisol.
Low cortisol (hypocortisolism) presents with severe fatigue and weakness, unexplained weight loss, low blood pressure causing dizziness, intense salt cravings, nausea and abdominal pain, depression and mood changes, and in primary adrenal insufficiency (Addison's disease), characteristic skin darkening. Addison's disease is a rare autoimmune condition affecting 40-110 per million people, requiring lifelong hormone replacement and carrying the risk of life-threatening adrenal crisis.
Chronic stress effects on adrenal function represent one of the most significant health challenges of modern life. Prolonged HPA axis activation (chronic stress) leads to physiological changes that contribute to immune dysfunction, metabolic disorders, cardiovascular disease, mental health conditions, and persistent fatigue.

Current medical understanding focuses on HPA axis dysfunction or dysregulation. This evidence-based framework recognizes that chronic stress can disrupt normal cortisol patterns and responses without necessarily indicating adrenal gland failure. Legitimate conditions like chronic fatigue syndrome/ME, burnout syndrome, and various autoimmune or endocrine disorders can cause similar symptoms and require proper medical evaluation and treatment.
How can hormone imbalances be treated?
Hormone imbalance treatment has evolved dramatically, with current approaches emphasizing evidence-based medicine, personalized care, and comprehensive lifestyle interventions alongside appropriate medical treatments.
Bioidentical Hormone Replacement Therapy (BHRT) uses laboratory-produced hormones that are chemically and structurally identical to those naturally produced by the human body. These hormones, derived primarily from plant sources like soy and yams, include estradiol, progesterone, and testosterone. BHRT can be delivered through multiple methods including pills, creams, gels, and more. The medical consensus emphasizes using the lowest effective dose for the shortest duration necessary, with individualized risk-benefit assessment for each patient.
Lifestyle interventions form the foundation of hormone balance and should be implemented alongside any medical treatments. Dietary approaches proven effective include consuming 25-30 grams of protein per meal to support peptide hormone production, increasing fiber intake to improve insulin sensitivity, incorporating healthy fats like omega-3 fatty acids, and following Mediterranean diet patterns that may help reduce estrogen levels and cancer risk while limiting processed foods and sugar.

Exercise plays a crucial role, with regular moderate exercise (150 minutes weekly) helping regulate cortisol and insulin while improving hormone receptor sensitivity. However, excessive exercise can decrease sex hormones and increase cortisol, highlighting the importance of balanced activity levels.
Sleep management is critical for hormonal health, requiring 7-9 hours of quality sleep nightly for proper growth hormone release and cortisol regulation. Poor sleep disrupts multiple hormones including ghrelin and leptin, contributing to weight gain and metabolic dysfunction.
Nutritional supplementation can support hormone balance when used appropriately. Evidence-based supplements include magnesium (150-300mg daily) for menstrual symptom relief and hormone production support, vitamin D3 with K2 for its hormone-like functions, omega-3 fatty acids for hormone production and inflammation reduction, probiotics for gut health and hormone metabolism, and adaptogenic herbs like ashwagandha for cortisol regulation and chasteberry for PMS relief.
Alternative and integrative approaches with scientific support include acupuncture and mind-body practices like tai chi, yoga, and meditation that support stress reduction and hormonal balance through cortisol regulation.

The field continues evolving rapidly with promising developments in personalized medicine, new FDA-approved treatments, and better understanding of lifestyle interventions. However, fundamental principles of evidence-based care, safety monitoring, and individualized assessment remain paramount for achieving optimal outcomes while minimizing risks.
Successful hormone balance treatment requires a comprehensive approach combining appropriate medical intervention when indicated, foundational lifestyle modifications, targeted supplementation based on individual needs, and regular monitoring with qualified healthcare providers familiar with current evidence-based guidelines.
If you have been experiencing symptoms that may be connected with hormone imbalances and are looking for answers, schedule a free consultation so we can talk about the appropriate lab testing and follow-up to restore your hormones to optimal levels to look and feel your absolute best.
